In a nutshell
- 🦠 Recurring infections and slow recovery: multiple colds back-to-back, sinusitis or chest infections that linger, repeated antibiotics, swollen glands and night sweats are red flags to discuss with a GP.
- 😴 Unusual fatigue and sleep changes: heavy, unrefreshing tiredness, brain fog and fragmented sleep; consider checks for iron, vitamin D, B12 and thyroid, while stabilising sleep timing and morning light exposure.
- 🧴 Skin, gut, and oral clues: eczema flares, slow-healing cuts, thrush, recurring mouth ulcers, frequent cold sores, and chronic gut upset may signal immune stress; support with good oral hygiene, emollients, and a fibre-rich, fermented-food diet.
- 🌥️ Seasonal and lifestyle factors: low winter vitamin D, dry indoor air, crowding, chronic stress and overtraining can tax immunity; prioritise steady movement, protein, zinc/selenium/omega-3, hydration, and moderate alcohol.
- 🛡️ Practical protections and when to seek help: use vaccinations (flu, COVID-19), handwashing and ventilation; seek medical advice if infections are unusually frequent, severe or prolonged, or fatigue doesn’t improve.
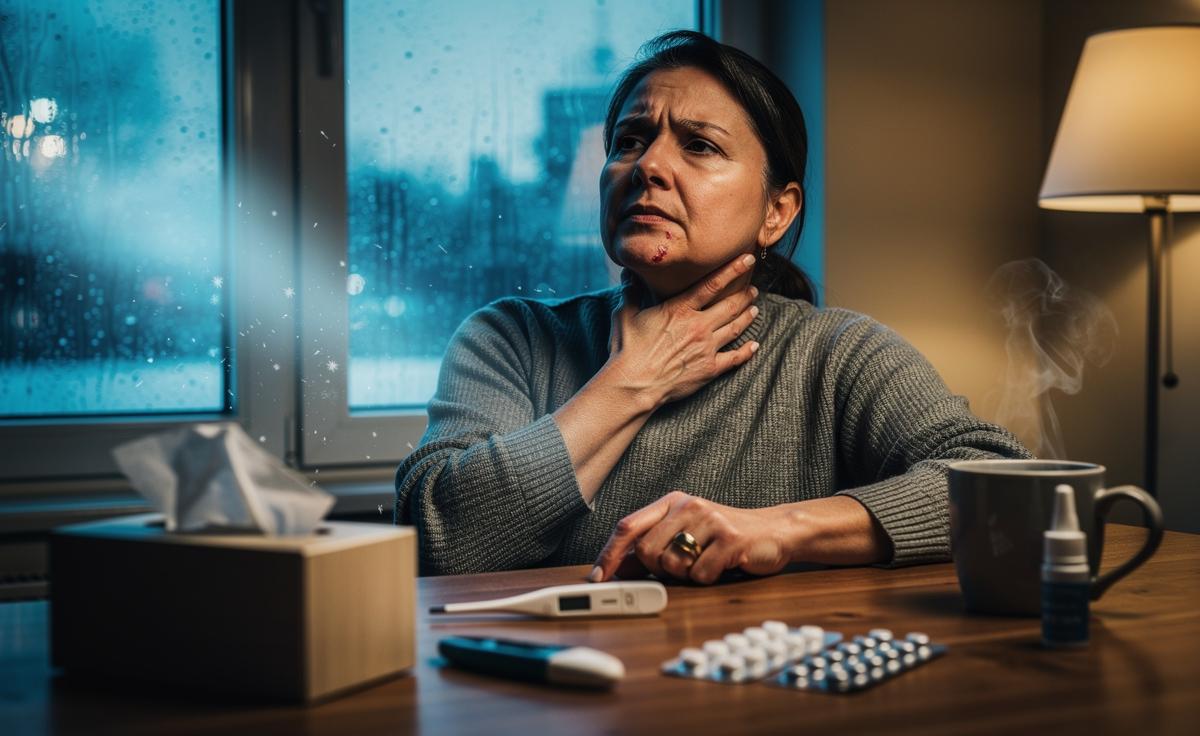
Winter has a way of surfacing chinks in our armour. As viruses swirl through classrooms, offices, trains and pubs, the difference between a robust immune response and a faltering one becomes obvious. Yet the clues are often subtle. A cough that never quite resolves. Mouth ulcers that keep returning. A deep, nagging tiredness you can’t sleep off. This guide lays out the tell-tale signs of a weak immune system and how to interpret them sensibly this season. If you notice several of these signals together, it’s worth pausing and reassessing your habits, risks and support. You don’t need to panic; you do need to pay attention.
Recurring Infections and Slow Recovery
One cold is normal. Two is common. But back-to-back infections that cling for weeks suggest immunity under strain. Look for patterns: recurrent sinusitis, frequent chest infections, earaches that return a fortnight later, or urinary tract infections that relapse despite treatment. Needing multiple antibiotic courses in a season is a red flag worth discussing with a GP. Equally telling is convalescence that drags. A cough three weeks on. Sore throats that fade, then flare. Wounds that take an age to knit. These slowdowns point to reduced immune efficiency, not just bad luck.
Fever behaviour matters, too. Some people mount low-grade fevers for days without decisive resolution; others barely raise a temperature at all. Neither is “wrong”, but both can hint at a system struggling to coordinate a response. Add in swollen glands that stay tender, night sweats, or breathlessness on minor exertion, and you have a pattern that merits attention. In children, persistent ear infections or unusually severe colds can be clues; in older adults, pneumonia risk rises when immunity dips. When infections become unusually frequent, prolonged or severe, treat it as data, not drama.
Unusual Fatigue and Sleep Disturbances
Not all exhaustion is created equal. Immune-related fatigue often feels heavy, unrefreshing, and indifferent to a full night’s rest. You may wake foggy, need naps you never used to, or find concentration slipping by mid-afternoon. Sleep itself may change: lighter, more fragmented, with early waking or restless legs. When sleep quantity stays the same but quality craters, the immune system frequently sits at the centre of the story. Low-grade inflammation alters sleep architecture and energy metabolism; the result is a body idling in the wrong gear.
Consider co-travellers. Recurrent headaches, muscle aches without a clear cause, or a subtle increase in resting heart rate can accompany immune strain. Post-viral dips are common after flu or COVID-19; many recover steadily, but some experience prolonged lassitude. Nutritional shortfalls—iron, vitamin D, B12—compound the slump, as do thyroid issues and unmanaged stress. The fix isn’t one note: consistent sleep timing, daylight exposure on winter mornings, protein-rich meals, and reducing late caffeine can nudge physiology back on track. If fatigue remains entrenched or worsens, involve your GP to rule out anaemia, thyroid disease or other drivers.
Skin, Gut, and Oral Clues
The body’s barrier tissues broadcast immune status in plain sight. Flaky, slow-healing skin, worsening eczema, or recurrent cold sores suggest local defences are flagging. In the mouth, thrush (creamy white patches), frequent ulcers, bleeding gums, or chronic bad breath can reflect disrupted microbial balance—often after antibiotics—or a broader immune wobble. When surfaces that usually protect you start to fail, investigate both local care and systemic health. In the gut, persistent bloating, diarrhoea or constipation, especially after infections, can signal a microbiome knocked off kilter. The knock-on effect: impaired nutrient absorption and a loop of further vulnerability.
| Sign | What It May Signal | Quick Action |
|---|---|---|
| Recurring mouth ulcers | Stress, B12/iron deficiency, mucosal immune stress | Check diet, consider blood tests, use saltwater rinses |
| Oral thrush | Antibiotic aftermath, inhaled steroid use, diabetes | Review medications, rinse after inhalers, seek antifungal if persistent |
| Cold sores flaring often | Immune dips reactivating HSV | Prioritise sleep, manage triggers, consider antiviral advice |
| Chronic gut upset | Post-infectious IBS, food intolerance, coeliac disease | Keep a symptom diary, trial soluble fibre, discuss tests with GP |
Simple steps help: regular brushing and flossing, alcohol-free mouthwash, and not overusing antiseptics that can strip helpful bacteria. For skin, gentle cleansers, thicker emollients in cold weather, and prompt care for cuts reduce infection risk. In the gut, a fibre-rich pattern—oats, legumes, vegetables, fermented foods—supports microbial diversity, and thus frontline immunity.
Lifestyle and Seasonal Risk Factors
Sometimes the “weakness” isn’t inherent; it’s imposed. Short days and indoor life trim our vitamin D levels, parching central heating dries airways, and crowded transport ups exposure. Chronic stress and skittish schedules amplify cortisol noise, blurring the immune system’s signals. Small, consistent habits beat heroic bursts in rebuilding resilience. Aim for regular movement—brisk walks, light strength work—while avoiding the trap of overtraining, which can transiently suppress defences. Prioritise seven to nine hours of sleep, ideally anchored by the same wake time daily.
Diet matters more than fads admit. Adequate protein supports antibody production; zinc, selenium and omega-3s help fine-tune inflammatory responses. A colourful plate is a practical proxy. Hydration supports mucosal barriers; alcohol, in excess, undermines them. Vaccinations—seasonal flu, COVID-19 boosters where appropriate—don’t make you bulletproof, but they do lighten the blow. Handwashing remains unfashionably effective; so does ventilation, even a cracked window on a packed bus. If you’re immunocompromised or caring for someone who is, speak to your GP or pharmacist about targeted protections during high-circulation weeks.
Put simply, your body leaves breadcrumbs. Frequent infections, stubborn fatigue, and shifts in skin, gut and oral health often point towards a taxed immune system. None of these signs alone seals a diagnosis; together, they sketch a picture you can act on. Tighten the basics, track patterns, and seek professional guidance when the dots start to join. The goal isn’t fear—it’s foresight. As the season unfolds, what signals is your body sending, and which small, steady changes could help you meet winter on the front foot?
Did you like it?4.5/5 (28)